Abstract

Patients with hematological diseases receiving an anti-CD20 monoclonal antibody, such as rituximab or obinutuzumab (R/Obi), show a low seroconversion rate after two doses of mRNA COVID-19 vaccines, especially if received within 12 months of their last R/Obi dose. The Centers for Disease Control and Prevention recommend booster vaccination at least three months after completing the primary series for immunocompromised patients. Although previous reports have shown that some non-responders achieved a humoral response after the third dose, the seroconversion rate was approximately 20%. In these studies, the interval between booster vaccination and the last R/Obi dose was shorter than six months, suggesting that the unsatisfactory seroconversion rate may be due to a lack of B cell recovery. In Japan, a third dose was offered seven months after the second vaccination, regardless of the immunosuppressive status, in early 2022. Booster vaccination at longer intervals may induce a higher humoral response rate in patients recently treated with R/Obi. However, only a few studies have examined this issue. In addition, the data on T cell responses after booster vaccination in these patients are limited. Therefore, this study aimed to investigate the humoral and cellular reactions of R/Obi receivers to mRNA COVID-19 vaccines, which were administered at an interval longer than that in Western countries.
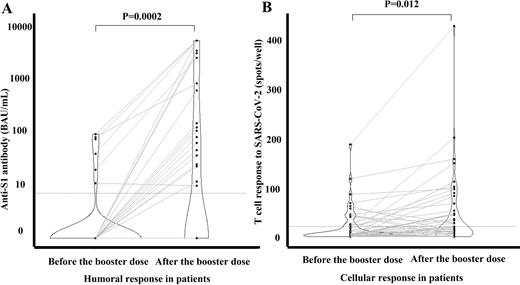
This study included 68 patients with hematological diseases who had received the primary vaccine series within 12 months of their last R/Obi dose and 30 healthy volunteers. Blood samples were collected before and 14-90 days after the booster vaccination. We set the primary endpoint as the proportion of subjects acquiring IgG antibodies to the S1 subunit of the spike protein of SARS-CoV-2 (anti-S1 IgG antibody; Abbott, Sligo, Ireland) with a range of 7.1-5,680 binding antibody units per mL (BAU/mL). Seropositivity was defined as anti-S1 IgG antibodies >7.1 BAU/mL. As secondary endpoints, we also evaluated the T cell response to SARS-CoV-2 in patients using an enzyme-linked immunospot assay (T-SPOT. COVID, Oxford Immunotec), with positivity defined as more than 20 spots/well.
Fifty-two patients (median age 73 years) whose data were available for analysis after data collection and 30 volunteers (median age 32 years) were included in the analysis. Twenty-one (40%) patients were diagnosed with diffuse large B-cell lymphoma, 16 (31%) with follicular lymphoma, 14 (27%) with other B-cell neoplasms, and one with benign hematological disease. Forty-four (85%) patients were in complete remission (CR), two were not in CR, and six (12%) were on R/Obi maintenance therapy. The median time from the second to the third vaccination was 223 days. The seropositivity rate before the booster vaccination was 12% and 100% in patients and volunteers, respectively, with median anti-S1 IgG titers of 0 (interquartile, IQR 0-0) and 82 (IQR 47-143) BAU/mL, respectively. (Fig.1A) After booster vaccination, the seropositivity rates were 42% and 100% in patients and volunteers, respectively, with median titers of 0 (IQR 0-89) and 2,504 (IQR 1,376-3,121) BAU/mL, respectively. (Fig.1A) The T cell response before booster vaccination was observed in 13 (25%) patients, all of whom were seronegative. (Fig.1B) After booster vaccination, it was detected in 22 (42%) patients, including 13 seronegative patients. (Fig.1B) All six patients on maintenance therapy remained seronegative; however, two patients showed T cell response before and four after a third dose, respectively. In total, either humoral or cellular response before booster vaccination was identified in 37% of patients, which increased to 67% after booster vaccination.
Booster vaccination within a seven-month interval induced a humoral response in 42% of patients recently receiving R/Obi, and the T-cell response was identified and enhanced in some seronegative patients. Around 70% of patients showed humoral, cellular, or both response after booster vaccination. These results provide insights into the rational vaccination strategy.
Disclosures
Kondo:Asahi Kasei Pharmaceutica,Chugai Pharma, MSD Pharmaceutical, Dainippon Sumitomo Pharma, Otsuka Pharmaceutical: Honoraria, Research Funding.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal